Sustainable health financing
Financing is a core element of health systems and a key enabling factor in the ability of countries to achieve universal health coverage. As part of its focus on promoting resilient and sustainable systems for health, UNDP works with partners to support investment strategies, national policies and regulatory frameworks to strengthen financing and public financial management for health.
Despite significant increases in domestic financing to address HIV and other health challenges in the last few years, many countries remain heavily dependent on external funding sources. As countries work to achieve the ambitious targets set by the 2030 Agenda for Sustainable Development, the sustainability of financing for health has gained increasing attention as a priority issue for sustainable development. Transforming health systems to achieve the SDG 3 targets is estimated to require an additional US$371 billion per year by 2030, for 67 low- and middle-income countries (LMICs), which make up 95 percent of the total population in LMICs.
The design and implementation of health financing policies influence the extent to which health systems can deliver quality health services, equitable utilization of resources, and financial protection for vulnerable populations. While domestic resource mobilization is one key dimension of sustainable financing, economic growth does not guarantee increased national budget allocations for health, nor do increased health budgets ensure that available resources for health reach the populations who need them most.
Strengthening financing for health calls for a holistic focus that prioritizes improvements to the efficiency and strategic use of existing resources as much as efforts to generate revenue, both domestic and international, in alignment with national development strategies. This includes the integration of health into national budgets for development, innovative financing and co-financing approaches, understanding and addressing co-morbidities, strengthened governance, and ensuring appropriate focus on key populations and synergies with other development objectives.
Context
Strong economic growth over the past two decades has resulted in more countries transitioning from low- to middle-income status. Amid broader trends of declining official development assistance (ODA) flows, external aid for health peaked in 2014 but has remained stagnant since 2015. Although government health spending grew between 2000 and 2018, with global spending on health reaching $8.3 trillion in 2018, it was slower than in recent years.
Prior to the COVID-19 pandemic, strained national budgets and reduced external support limited government capacities to expand health services towards the achievement of universal coverage, particularly in low-income countries. Global HIV/AIDS spending has remained flat for years, after peaking in 2013, compounding challenges for countries previously dependent on development assistance for their disease response (UNAIDS, Resources and financing, 2021).
The economic shocks triggered by the COVID-19 pandemic, coupled with the devastating impact on health systems, have exacerbated previous health financing vulnerabilities. The global gross domestic product loss due to the COVID-19 pandemic in 2020 was estimated to be approximately $4 trillion. Deep economic contractions in donor countries threaten the external financing flows to lower income countries, for which aid makes up nearly 30 per cent of health spending on average. The growing needs for health services amid the health crisis combined with a more fiscally constrained environment threaten to reverse progress on universal health coverage and widen existing health inequities (WHO, Global Health Expenditure Report, 2020).
The multiple channels through which health financing can align with and contribute to SDG implementation is reflected in the measures that countries have prioritized in the Addis Ababa Action Agenda, the global framework for financing sustainable development.
The Agenda highlights, for example, opportunities for health financing strategies to:
- Support the mobilization and effective use of domestic public resources: leveraging tobacco taxes as an additional revenue source and means of reducing health care costs; increasing public expenditure to ensure universal health coverage; and scaling investments in NCDs;
- Unlock private investment from domestic and international sources: private investments must protect health standards and be aligned with public health goals;
- Scale international public finance: more countries need to work towards innovative sources and mechanisms of additional financing, based on models combining public and private resources. Public-private partnerships for health like Gavi and the Global Fund make a significant contribution to financing the SDGs based on this model;
- Tap into international trade as an engine for development: trade agreements like the WTO Trade, Intellectual Property Rights and Access to Medicines (TRIPS) agreement can be leveraged to facilitate improved access to affordable essential medicines for developing countries.
What does sustainable health financing entail?
The design and implementation of health financing policies influence the extent to which health systems can deliver high-quality health services, equitable utilization of resources, and financial protection for vulnerable populations. While domestic resource mobilization is one key dimension of sustainable financing, economic growth does not guarantee increased national budget allocations for health, nor do increased health budgets ensure that available resources for health reach the populations who need them most.
Strengthening financing for health calls for a holistic focus that prioritizes improvements to the efficiency and strategic use of existing resources as much as efforts to generate revenue, both domestic and international, in alignment with national development strategies. This includes the integration of health into national budgets for development, innovative financing and co-financing approaches, understanding and addressing co-morbidities, strengthened governance, and ensuring the appropriate focus on key populations and synergies with other development objectives.
Beyond ensuring there are sufficient resources to support the full functioning of the health system, sustainable health financing also refers to the efficacy of such funding in protecting the population from financial risks in accessing the health services they require. A key role for sustainable health financing is thus to support health systems to achieve universal health coverage by reducing health inequities and minimizing financial hardship on the poor.
As defined by the World Health Organization (WHO), health financing consists of a range of functions, including revenue raising, pooling and purchasing, as well as policies relating to service benefits to which some or all of the population are entitled. The entry points to improving the sustainability and impact of health financing are numerous, necessitating a combination of approaches at both the policy and programme levels. They entail considerations for, inter alia, budgeting frameworks, the design of benefit packages for health, social protection and health insurance frameworks, including community-based health insurance and free health care policies, resource-tracking and revenue-raising, fiscal space for health and public health taxes.
Among the key cross-cutting areas for improved health financing is that of public financial management (PFM). A strong PFM system – the institutions, policies and processes that govern the use of public funds – can ensure higher and more predictable budget allocations, reduced fragmentation in revenue streams and funding flows, timely budget execution and better financial accountability and transparency.
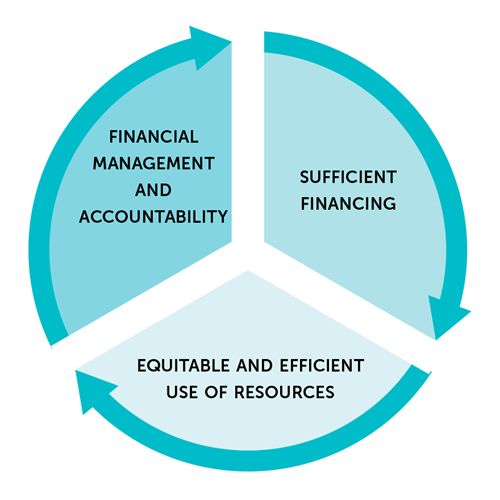
Given that public funds are the cornerstone of sustainable health financing in most countries, WHO underscores the central role for systems as a key enabling factor to achieve universal health coverage. A strong PFM system – the institutions, policies and processes that govern the use of public funds – can ensure higher and more predictable budget allocations, reduced fragmentation in revenue streams and funding flows, timely budget execution, and better financial accountability and transparency.
UNDP’s approach
Among the action areas which UNDP focuses its policy and programme support for health and development, as outlined in its HIV and Health Annual Report 2020-2021, sustainable health financing is a priority area through which UNDP promotes effective and inclusive governance for health. This cross-cutting policy focus complements and reinforces UNDP’s support to national partners in implementing large-scale health programmes in challenging operating environments, as part of UNDP provides technical assistance and capacity building to strengthen frameworks and processes for financial management.
UNDP service offerings for sustainable health financing include policy and programme support on:
- improving efficiencies, including allocative efficiencies, for HIV and health;
- innovative approaches to sustainable HIV and health financing, including developing investment strategies and national investment cases using a rights-based approach and leveraging other activities such as social contracting of civil society organisations to increase domestic financing for health.
UNDP also engages in global and regional processes and partnerships that contribute to sustainable health financing. In the Joint United Nations Programme on HIV/AIDS (UNAIDS) Division of Labour, UNDP is co-convener with the World Bank for the “Investment and Efficiency” thematic area.
Beyond HIV and health, UNDP plays a lead role in promoting financing solutions for sustainable development, as part of its mandate to support SDG implementation. UNDP provides knowledge leadership to contribute to the evidence base on sustainable financing and help countries identify and implement catalytic approaches. The online platform ‘Finance Sector Hub’ discusses UNDP’s tools and broader support to sustainable SDG financing.
Tools and approaches
UNDP, together with partners, supports sustainable health financing through a diversity of approaches, including those to generate revenue, avoid future expenditures, deliver better, and realign expenditures. Its aim is to enhance the sustainability and impact of health financing systems. Within its focus on promoting the mobilization and effective use of domestic public resources, UNDP provides support to countries by modelling optimized investment approaches, promoting affordable access to medicines and advising on transition processes related to domestic financing of national disease programmes .
Modelling optimized investment approaches
Working in close partnership with key partners, including the World Health Organization (WHO), other United Nations agencies, the World Bank, the Global Fund to Fight AIDS, Tuberculosis and Malaria (The Global Fund) and the STRIVE Research Consortium of the London School of Hygiene and Tropical Medicine, UNDP develops investment cases and conducts modelling to help countries identify the most effective investment strategies and efficient use of technical and financial resources.
This includes:
- Promoting cross-sectoral co-financing approaches to increase the allocative efficiencies of investments in health and development: UNDP helps to identify investment opportunities in high-value interventions that deliver benefits across multiple development targets simultaneously, with benefiting sectors pooling their resources to finance these opportunities jointly.
- The declaration of the third high-level meeting of the General Assembly on the prevention and control of non-communicable diseases: the Addis Ababa Action Agenda notes the enormous burden that non-communicable diseases (NCDs) place on both developing and developed countries. Increased investments in preventing NCDs, for example through excise taxes on health-harming products, can reduce public and private health-care costs while raising revenue and delivering wider societal benefits, such as reduced poverty and increased productive capacities.
- Advancing multisectoral action for tobacco control, including for raised tobacco excise taxes as part of the World Health Organization (WHO) Framework Convention on Tobacco Control investment cases: these cases provide evidence of the return on investment for countries of raising tobacco taxes to reduce tobacco consumption and the related social and economic costs. They also assess the revenue-generating potential of these taxes and provide recommendations on the efficient allocation of that revenue to domestic health budgets and pro-poor investments.
Promoting affordable access to medicines
Ensuring affordable and fair pricing of medicines through effective health financing mechanisms is a key enabling factor for achieving universal health access. UNDP helps countries to review policy options and approaches to the pricing of essential medicines, including through the development of a price comparison tool as part of its work under the Access and Delivery Partnership.
UNDP supports governments to purchase good-quality medicines at the best price through its health procurement support. In Ukraine and Kazakhstan, for example, UNDP support on pricing negotiations helped the governments to achieve breakthrough price reductions in cost of treatment for hepatitis C, a significant step towards increasing access to medicines. Through the review of legal and regulatory frameworks related to the procurement of antiretroviral medicines, UNDP also helps to optimize efficiencies and ensure access for populations at higher risk of HIV infection.
Trade policy represents another pathway through which countries can reduce the cost of medicines to better meet the goal of universal access. UNDP provides advisory services to countries related to the World Trade Organization (WTO) Agreement on Trade Related Aspects of International Property Rights (TRIPS), which includes a number of flexibilities that can be used to reduce the prices of essential medicines.
Advising on the transition processes related to domestic financing of national disease programmes
As more countries assume middle-income status and transition away from externally funded health programmes, particularly for HIV, it is critical that they develop sustainable financing strategies using domestic resources, taking into account the need to scale up service coverage, as well as service quality and efficiency. An important strategy for many countries is social contracting of non-governmental organizations (NGOs) as providers of HIV-related and other health services, which can help to facilitate effective service delivery and efficient use of domestic resources. UNDP helps countries to tap into this mechanism by analysing legal frameworks and providing policy recommendations to governments on social contracting. UNDP also provides thought leadership and support to countries and partners on better understanding and addressing co-morbidities to increase allocative efficiencies.
While increased availability and strategic use of domestic public resources are critical to financing universal health coverage, even with projected increases in domestic health spending, a US$20-US$54 billion annual funding gap would remain. UNDP’s support to identify innovative financing for health therefore includes a focus on helping countries unlock private capital and tap into international financial assistance, complementary to domestic public resources. This includes:
- Supporting the development and operationalization of social impact bonds to leverage private capital for health: UNDP is conducting a feasibility study in Zambia to inform the first ever tobacco-control social impact bond. The study will use a results-based model to examine the social, financial and environmental benefit to countries of their transitioning away from tobacco cultivation toward alternative crops/livelihoods for farmers who want to transition.
- Tapping into financing opportunities at the nexus of health and environment: UNDP is currently conducting a feasibility study in Namibia, for example for its Solar for Health initiative, with the aim of increasing private sector investment.
Beyond HIV and health, UNDP plays a lead role in promoting financing solutions for sustainable development, including through knowledge-sharing. The online platform “Finance Sector Hub” discusses UNDP’s tools and broader support to sustainable SDG financing.
Key resources
UNDP Finance Sector Hub for Sustainable Development Goals
This is a UNDP database of financing solutions that provide strategies and means to effectively unlock and direct sources of finance toward realising the SDGs.
Website

World Health Organization’s Health Financing Resources
Read more about health financing topics such as voluntary health financing, performance-based financing and revenue raising.
Website
